Central Venous Catheter: A Lifeline for Patients in Critical Care
 |
| Central Venous Catheter |
Central venous catheters (CVCs) play a vital role in
modern healthcare. They allow access to the large vein structures close to the
heart for purposes such as fluid administration, blood drawing, and medication
delivery. This direct vascular access is critically important for patients
requiring intensive care, complex surgeries, chemotherapy, total parenteral
nutrition, or long-term antibiotic therapy. Without CVCs, it would be extremely
difficult or impossible to deliver these intricate treatments successfully.
Types of Central Venous Catheters
There are different types of CVCs based on their intended use and duration.
Short-term, non-tunneled catheters are most commonly used in the hospital
setting for procedures and acute care needs lasting days to weeks. These
include peripherally inserted central catheters (PICCs) and internal jugular or
subclavian catheters. Tunneled catheters have cuff anchors that allow them to
remain in place for weeks to months. Implanted ports offer lifelong access via
a port chamber just under the skin that connects to a CVC. They are utilized
for recurrent treatments like chemotherapy.
Catheter Placement and Maintenance
CVC insertion requires specialized skills and image guidance like ultrasound or
fluoroscopy for proper positioning in the desired central vein. Standard
sterile technique is followed to minimize infection risk. The catheter entry
site is secured and assessed regularly for redness or swelling during use.
Dressings are changed periodically, and the catheter hub is disinfected before
each access. Flushing with saline keeps the lumens patent. When no longer
needed, the catheter is removed aseptically to prevent complications. Proper
care and monitoring help maximize patient safety.
Cost Savings and Operational Efficiency
While initial Central
Venous Catheters placement
involves costs, it provides immense returns by allowing efficient delivery of
complex therapies. Multiple blood draws or IV lines are avoided, reducing
nursing time and supplies. Patients recover more rapidly from serious illnesses
or undergo long transplant waits comfortably at home with port access. This
decreases expensive hospital days and readmissions. CVC programs generate
significant cost savings annually for healthcare systems through optimized
resource use without compromising quality of care.
Challenges of Central Line-Associated
Infections
Despite strict protocols, CVCs carry a small but serious risk of central
line-associated bloodstream infections (CLABSIs). These occur in approximately
4 per 1,000 catheter days and extend hospital stays by weeks with added
antibiotic treatment costs averaging $45,000 per case. Zero tolerance policies
are in place at leading facilities through multi-disciplinary teams focusing on
education, monitoring, and rapid response. Introduction of antimicrobial
impregnated catheters has further lowered infection rates substantially.
However, more research into novel technologies, surface modifications, and care
bundles continues to be paramount. Even a single CLABSI has devastating human
and financial implications.
Role of Anesthesiologists and
Interventional Radiologists
The specialties of anesthesiology and interventional radiology (IR) are at the
forefront of CVC placement and programs. Anesthesiologists have long placed
CVCs during surgery or critical illness. Meanwhile, IR has advanced
image-guided techniques with real-time visualization of catheter passage
through veins. Their central line skills and expertise in vascular access
provide reliable options for difficult cases. Many catheterization laboratories
(cath labs) are now jointly managed by anesthesiology and IR departments to
streamline operations and standardize quality. This has synergized resources
for optimal CVC insertion services across various clinical settings.
Future Innovations
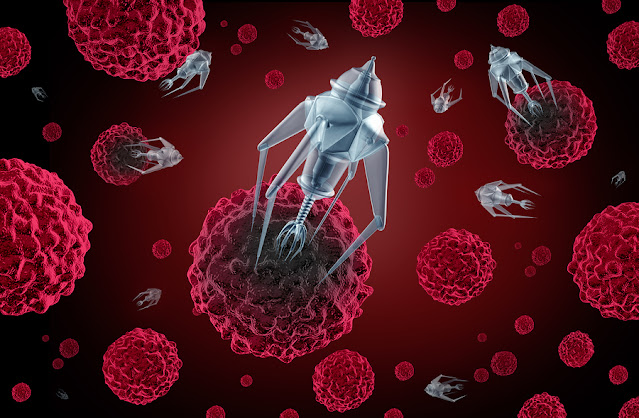
Novel catheter designs, surface modifications, and guidance technologies aim to
further evolve central line safety. Antimicrobial impregnations with longer
durability, rapid hemostasis valves, needleless securement devices,
infection-resistant materials, and biofilms continue enhancing function while
mitigating risks. Emerging techniques harness robotics, augmented reality, and
artificial intelligence to optimize placement accuracy and outcomes. Ports may
integrate additional monitoring capabilities. As multidisciplinary teams expand
capabilities through research and training, CVCs will continue empowering
life-saving therapies by accessing central circulation.
Get
more insights on This Topic- Central
Venous Catheters
Explore
More Articles –Storage
Basket Rack Market


Comments
Post a Comment