Blood Based Biomarker: The Future of Non-Invasive Disease Diagnosis and Treatment
 |
| Blood Based Biomarker: |
A biomarker is a measurable substance in the body that
can indicate the presence of a specific disease or condition. Over the years,
various biomarkers have been identified for many diseases through extensive
research. However, most traditional biomarkers require an invasive procedure
like tissue biopsy to measure. This poses challenges and limitations for wide
clinical use.
The Rise of Blood Based Biomarker
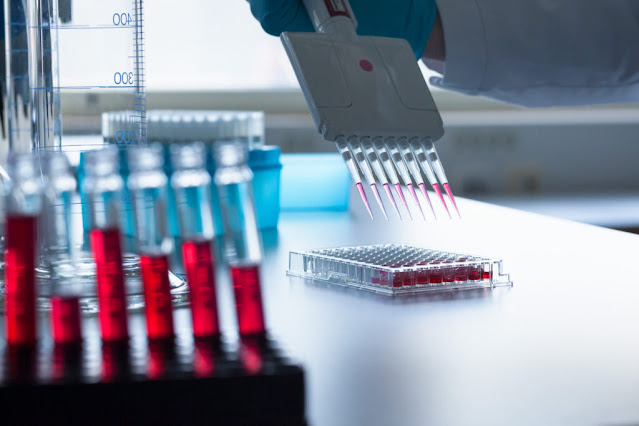
In recent years, researchers have begun exploring Blood
Based Biomarkers that can be measured through a simple blood draw.
Blood carries molecules and cells from throughout the body that can provide
clues about health conditions. The development of highly sensitive technologies
like proteomics, metabolomics and next-generation sequencing has enabled
detection of subtle changes in the blood that correlate with disease. Some key
advantages of blood-based biomarkers include their non-invasive nature, low
costs, and ability to serially monitor health over time.
Applications in Cancer Diagnosis and
Monitoring
Cancer biomarkers have seen some of the most significant advances with
blood-based approaches. Certain proteins, DNA fragments and exosomes released
by tumors can be detected in blood long before a cancer is detectable through
standard imaging. For example, drops in prostate-specific antigen (PSA) levels correspond
well with response to prostate cancer therapies. Researchers are also exploring
DNA methylation signatures and mutations present in circulating cell-free DNA
(ccfDNA) to detect over 50 cancer types with high accuracy. As costs decrease,
multi-cancer blood tests may transform early cancer detection. Serial blood
tests also allow close monitoring of disease recurrence and therapy response
without repeated invasive biopsies.
Cardiovascular Disease Risk Assessment
Biomarkers play a major role in cardiovascular disease (CVD) risk
stratification and management. Traditional markers like HDL, LDL and hs-CRP
levels are routinely measured. Emerging blood tests analyze over 200 lipid
metabolites and proteins linked to atherosclerosis development and plaque
rupture. They provide a more detailed risk score by incorporating factors like
inflammation, oxidative stress and insulin resistance beyond traditional risk
factors. Some blood tests can also detect early signs of heart damage within 3
hours of a heart attack to guide prompt treatment. As CVD remains the leading
cause of death, such advanced blood tests are driving more personalized
prevention and intervention strategies.
Neurodegenerative Disease Diagnosis
Alzheimer’s and Parkinson’s diseases cause significant disease burden
worldwide. Currently, accurate diagnosis requires brain imaging or autopsy, too
late for therapeutic intervention. Blood-based biomarkers show promise for
preclinical detection and disease monitoring. Researchers have identified abnormal
levels of amyloid-beta, tau, alpha-synuclein and other neuronal proteins in
plasma that correlates well with presence and stage of neurodegeneration. Some
studies report detection up to 20 years before symptom onset. On-going
validation in large cohorts may result in minimally invasive blood tests to
reliably diagnose, track progression and measure treatment responses for these
currently incurable conditions.
Non-Alcoholic Fatty Liver Disease Risk
Prediction
Non-alcoholic fatty liver disease (NAFLD) affects one in three adults globally
and often progresses to liver cirrhosis. It is now a leading cause for liver
transplantation. Early detection through regular blood tests and lifestyle
changes can help slow disease progression. Circulating levels of liver enzymes,
adipokines and other metabolic biomarkers have demonstrated utility in
identifying patients at higher risk of advanced liver fibrosis requiring
biopsy. As NAFLD becomes more prevalent with rising obesity rates, widespread
application of accurate blood-based risk prediction models may help focus
medical resources on those in greatest need of interventions like weight loss
or pharmacological therapies.
Utility in Drug Development and Precision Medicine
Blood-based biomarkers have found broad applications in pharmaceutical research
and clinical practice. They allow non-invasive monitoring of drug metabolism,
target engagement, safety and efficacy during clinical trials using smaller
sample sizes. Serial blood testing for biomarkers can rapidly identify
effective therapies and discontinued ineffective treatments. Their use promises
to revolutionize drug development and propel the future of precision medicine
where treatments are tailored based on an individual’s biomarker profile. As
biomarker discovery accelerates, regulatory agencies have provided clear
pathways for their clinical validation and qualification for risk assessment,
diagnosis and treatment decision making.
Blood based biomarker are transforming disease diagnosis, risk prediction,
monitoring and drug development. Their non-invasive nature, relatively low
costs and ability to uncover pathological changes in early, pre-symptomatic
stages offer immense potential to improve clinical outcomes and quality of
life. Combining proteomic, metabolomic and molecular signatures may yield
highly accurate multifactor disease risk scores and response predictors. As
technologies continue advancing, blood tests have the potential to redefine
standards of care across various therapeutic areas over the next decade.
Get
more insights on This Topic- Blood
Based Biomarker


Comments
Post a Comment