Anticoagulants: Understanding The Important Role Of Blood Thinners
 |
| Anticoagulants |
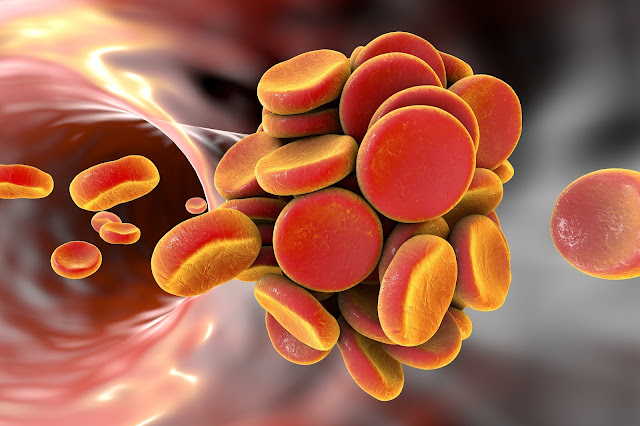
Blood clotting, also known as coagulation, is an
important process in our body that helps stop bleeding from cuts or wounds.
However, uncontrolled or excessive clotting can lead to dangerous medical
conditions like heart attacks, strokes or pulmonary embolism. This is where
anticoagulants, commonly known as blood thinners, play a crucial role by
preventing or treating such clot-related complications. In this article, we
explore various aspects of anticoagulants - their uses, types, effectiveness
and safety considerations.
Uses of Anticoagulants
Anticoagulants are prescribed by doctors for a number of medical conditions where
preventing clots is necessary. Some of the major uses of anticoagulants
include:
Atrial Fibrillation: Irregular heartbeat or atrial fibrillation increases the
risk of blood clots forming in the heart's upper chambers. Anticoagulants are
prescribed to reduce this risk and prevent stroke.
Deep Vein Thrombosis (DVT): Blood clots in the leg veins, called DVT, can
dislodge and travel to the lungs causing a potentially fatal blockage called
pulmonary embolism. Anticoagulants are given to prevent recurrence of DVT.
Heart Attacks and Stents: Clotting during or after a heart attack can further
damage the heart tissue. Blood thinners are prescribed after heart attacks and
procedures like stent placement to prevent clots.
Hip and Knee Replacements: Joint replacement surgeries increase the risk of
blood clots in the legs. Anticoagulants are prescribed for 4-6 weeks after such
surgeries to reduce clot risks.
Types of Anticoagulants
Based on their mechanisms of action, anticoagulants can be broadly classified into
two categories:
Vitamin K Antagonists: Warfarin was the first oral anticoagulant discovered and
remains an important option. It works by interfering with vitamin K which is
required for blood clotting. Other examples include phenprocoumon and Anticoagulants.
Direct Oral Anticoagulants (DOACs): Developed since the 1990s, DOACs like
apixaban, rivaroxaban, dabigatran and edoxaban directly target specific
clotting factors in the blood. They have predictable effects and do not require
frequent monitoring.
Different anticoagulants have their pros and cons in terms of effectiveness,
safety, drug interactions and monitoring needs. Doctors choose the right one
based on individual patient factors, medical condition and lifestyle.
Effectiveness of Anticoagulants
Clinical trials have demonstrated the effectiveness of anticoagulants in
reducing health risks associated with clotting:
Stroke Prevention: Several studies found that warfarin reduces stroke risk in
atrial fibrillation by approximately two-thirds compared to placebo. DOACs are
non-inferior or superior to warfarin for stroke prevention.
DVT Treatment and Prevention: Anticoagulants significantly reduce recurrent DVT
and potential life-threatening pulmonary embolism as compared to placebo or no
anticoagulation after an initial clot event.
Heart Attacks and Stents: Long-term use of blood thinners post heart attack and
stenting has been shown to cut chances of re-occurrence by approximately
one-third.
Hip and Knee Surgery: Meta-analyses of clinical trials showed that
anticoagulants lowered risk of DVT by approximately 80% and pulmonary embolism
by 60% after orthopedic surgeries.
Overall, anticoagulants have well-established efficacy in preventing thrombosis
and re-occurrence when used as per recommended treatment durations and dose
levels tailored to individual patients. However, safety must also be carefully
monitored.
Safety Considerations for Anticoagulants
While anticoagulants are highly effective, they also increase the risks of
bleeding because of their blood thinning effects. The main safety
considerations are:
Bleeding Risks: All anticoagulants increase chances of internal bleeding in the
brain, stomach, gastrointestinal tract and other organs. This risk is greater
in elderly population and with certain drug interactions or comorbidities.
Monitoring Needs: Warfarin needs regular prothrombin time (PT/INR) monitoring
and dose adjustments based on results to maintain safety and effectiveness.
DOACs have more predictable effects but monitoring may still be needed in
certain cases like impaired kidney function.
Drug & Diet Interactions: Warfarin response can be affected by various
drugs as well as foods high in vitamin K. DOACs have fewer interaction concerns
but still require caution with certain medications that use the same
elimination pathways.
Temporary Discontinuation: Guidelines recommend stopping anticoagulants before
many surgeries, dental procedures or injuries due to increased bleeding risks
during healing periods.
Overall, when taken as prescribed under medical supervision with caution
regarding potential interactions and risks of high intensity periods,
anticoagulants have a good safety profile. But unintended breaks or incorrect
dosing may reduce their benefits.
Managing Anticoagulant Therapy Safely
Given their risks, it is important for patients as well as healthcare providers
to effectively manage anticoagulant therapy. Some key measures include:
Complying with Prescribed Dosing: Patients should follow instructions on exact
drug, dose, schedule and duration and report any missed doses to doctors.
Non-compliance can cause under-anticoagulation as well as increase bleeding
risks.
Lifestyle Modifications: Patients should avoid potentially risky activities
like contact sports. Dietary restrictions may apply depending on the
anticoagulant prescribed. Alcohol and supplements should only be taken under
medical guidance.
Monitoring: Periodic blood tests help monitor effects of warfarin therapy
precisely for safety and adjusting doses if needed. For DOACs, impaired kidney
function warrants closer monitoring. Any signs of excess bleeding also requires
prompt medical assessment.
Recording Medications: Patients should maintain accurate lists of all
prescribed drugs, OTC medications, supplements to share with every doctor
systematically for checking potential medication interactions.
Emergency Identification: Medicalert bracelets or cards help alert emergency
responders to special medical needs. Ambulance services and nearest hospital
should also be informed in advance about anticoagulation use.
Get
more insights on- Anticoagulants
Check more
trending articles related to this topic: Trypsin


Comments
Post a Comment